The human body's detoxification process is a chemical masterpiece in human development where removing toxins is not just a matter of physically shifting them. In fact they do not shift unless they are first altered chemically. The chemical alteration is carried out by specific enzymes which require nutrients for their action. Some of the nutrients are needed to ensure that enough of these enzymes will be formed, some are needed as co-factors for the reaction and still others are raw materials needed for the transformation of the toxins. The point is that the biochemical mechanisms are known and the nutrient requirements can be defined. This article sets out details of the nutrients required at a cellular level to put this detoxification process into effect.
"Today, those who grasp the principles of natural medicine are keener than they ever have been about the detoxifying process of the body.
They are more acutely aware than past generations that chronic illnesses are promoted by toxins in the tissues and that these cause damage to the delicate structures of the living cell".
1 The Naturopathic Idea of the Detoxification Process

The early naturopaths were enthusiasts for detoxification of the body long before biochemists had any real idea of the nature of the detoxification process. Some of them even stretched back before the days when biochemists were first heard of. After all, the first biochemical laboratory was set up at Cambridge in the UK by Sir Frederick Gowland Hopkins in the early part of the 20th Century. These naturopaths were enthusiasts for grapefruit "fasts", out and out fasting, enemas and colonic irrigation, Epsom salt baths, internal castor oil and castor oil packs and poultices and hydrotherapy. None of this ever seemed to receive any scientific validation or, indeed, any scientific investigation.
The naturopaths were "people of insight" rather than biochemists or experts. Even the best of them undoubtedly worked on the basis of a lot of intuition supported by a considerable skill in the observation of patients, with an ability to evaluate their own results in naturopathic terms.
Science and naturopathy have often been in conflict. In particular scientists accused naturopaths (on the rare occasions when they deigned to recognize their existence at all) of pontificating about toxins without knowing to what they were referring and talking about detoxification without any understanding of the nature of the process. Of course, the scientists were quite right - that was what was happening. But many of the naturopaths were men and women of insight and intuition and they could genuinely read into their observations on patients subtle and beneficial changes when the measures that naturopaths called "detoxifying" were put into effect. In short, they had a conviction that their methods were working. Today we can put the two fields of knowledge together and largely wipe away the conflict. Most medical scientists are not yet ready to take part in that process but we can do it anyway because we can use the publications of research scientists and see how they are compatible with and, indeed, without intending to be, supportive of the naturopathic position.
2 Popular Understanding of Detoxification Processes Today
In respect of all fields of nutrition and naturopathy, this author finds it necessary to keep reminding readers and students to focus upon the living cell. Intoxication and detoxification are essentially phenomena of each and every living cell in the body. This is the fundamental biochemical level. It makes sense to look at that level. Too often people today have too gross and simplistic an idea of what detoxification is. Having had a bowel movement they may say "I have had an elimination". Whilst this is bound to be true in one sense because they have eliminated some contents from the bowel, it leaves an open question as to whether or not any cellular elimination has taken place.
We keep eating. The food and food residues have to pass along the alimentary tract. Eventually they must emerge at the other end. That is all unremarkable. However, as the food residues pass along the intestines they may have putrefied and thereby added to the toxic load of the body. Alternatively these residues may have avoided putrefaction and taken up significant toxins that were being voided in the bile. In that case the passing out of the waste does represent a true elimination of some small part of the body's toxic burden.
The true process of detoxifying begins within the living cells. Each cell of the body has to defend itself by resisting the uptake of toxic substances and by striving to detoxify and dispose of those toxins. If the individual cells of the body can do that and the main organs of elimination (liver and kidney) can remain un-compromised, then the flow of toxins to the exterior can be maintained.
Indeed, the activity of the cells of such organs as liver and kidney is crucial, for these organs must bear the brunt of the work of externalizing the toxins. Failure to envision detoxification as a cellular process is what is responsible for the common over-simplistic view. It is the failure to distinguish the bowel movement itself (which may be of little or no significance) from the toxic load that the bowel movement may or may not carry away.
3 Bowel Cleansing
The herbal bowel cleanse is popular among those who have gained naturopathic understanding. Many people think of a bowel cleanse as a detoxification. That idea cannot be entirely wrong because the bowel is often a prime source of body toxicity, harbouring long-standing food residues that generate toxins under the influence of an adverse bowel flora. Such toxins are absorbed and become part of the whole body toxic burden. Removing such residues therefore removes an important toxin source. In suitable cases, once this source is removed and the body is no longer under attack from constantly renewed supplies of the toxins, the body may cope better with the rest of its toxic load and you have health improvement. This is well known and it is what the bowel cleanse is all about.
However if the other main organs of elimination, the liver and the kidney most particularly, are already too compromised with toxicity, then no such improvement may occur. They themselves are too heavily burdened to accept the opportunity that the bowel cleanse presents. They remain sluggish and cannot make progress in voiding the body's toxins.

"To detoxify the body we must achieve cellular elimination, that is, we must encourage the cells of the liver, kidney and other organs to both detoxify and then externalize their toxic content"
By observing this we can see that elimination from the bowel is doing only one part of the job. To detoxify the body we must achieve cellular elimination, that is, we must encourage the cells of the liver, kidney and other organs to both detoxify and then externalize their toxic content. This means that although a bowel cleanse alone may often be of help, to do a full job one must take other action designed as a specific encouragement of cellular detoxification.
4 The Nature of The Cellular Detoxification Process
To many people, "detoxification" may be a vague term associated only with "getting rid of toxins" however, biochemists are quite clear about what it means and know that it involves converting the toxins into something else. Detoxifying toxins usually requires two steps. The first is chemical transformation of the toxin, usually by oxidation, by which it is converted to another substance, a derivative of the original toxin. The second is conjugation, which means attaching the toxin derivative to another molecule (called a "ligand") to render it much less toxic. The first step is conducted by enzymes known as Phase I enzymes, while the second step is conducted by Phase II enzymes. Each of these groups of enzymes has specific co-factors required for the enzymic reaction to proceed and many of these are available only through good nutrition. For Phase II you need a supply of the ligands that have to be attached. If one wants to take action to encourage these detoxifying enzymes then the way forward is to put together all the principal nutrients that these enzymes need and to make sure to consume enough of each type. Of course it also make sense to avoid all avoidable toxin intake since retoxifying during an effort to detoxify will be counter-productive. That step translates into a separate effort to optimize the diet and the environment for toxin reduction. Here though, we focus upon the special nutritional needs of the detoxifying enzymes. There are two very good literature sources for this topic, Parke et al (1993a) and Institute for Functional Medicine Inc. (1999).
5 The Myth of Fasting
Fasting is a method that was popular among the older naturopaths for inducing the bodies detoxification process and a good many of today's adherents retain this practice. By fasting one means complete withdrawal of food while continuing to supply as much water as required. It is, therefore a complete withdrawal of nutrient input. Variants, such as the grapefruit fast mentioned above, or the rice fast, are only partial fasts. If the water used contains significant dissolved nutrients then that too would break a true fast. It was thought that fasting would accelerate detoxification because it was a way to interrupt the inflow of fresh toxins from the environment. Those toxins that normally accompany food would be interrupted. Moreover, they considered that the energy normally devoted to digesting and assimilating food could be redirected into the energy needs for detoxification.



The logic of this approach seems compelling at least until one realizes that detoxification requires nutrients and there has to be a balance between the benefits outlined above and the inevitable depletion of nutrients that marks the onset of starvation. Certainly it seems that any fast that one undertakes in order to encourage detoxification should be strictly limited in its duration. This writer, in his role as a practitioner, chose never to employ fasting. The main reason for that is the depletion in anti-oxidant nutrients that starts to occur as soon as food is withdrawn. The price we pay for that is that the cell structure and cell enzymes are at once at increased risk from free radical damage. With free radical damage being an important mechanism, if not the primary mechanism by which cell damage occurs, this ought to make one think twice about the merits of fasts, (Blake et al 1987, Lunec 1990). The early naturopaths obviously had no access to such information upon the rates of free radical damage. It is easy to draw from this the conclusion that the boost to detoxification through fasting must be very short-lived. At worst it is open to question whether the boost exists at all. As fasting proceeds, we suffer a drop in the tissue levels not only of externally derived antioxidants like carotenoids and flavonoids but also of important internal tissue co-factors like glutathione.
6 Diets to Facilitate the Detoxification Process
In nutritional practice it has become clear that effective detoxification can and does take place while continuing to eat. It is very important that this should be so because detoxification of the body toxin burden can never occur in a short space of time. The older naturopaths, for all that we owe them in developing the naturopathic philosophy, were often in error in thinking that much good could be done through short-term "splurges" of detoxifying effort. This was encouraged by the situation that applied in health farms and hydros, where health-seeking visitors were only available for a week or a fortnight at a time. Little can be achieved in the short term. Rather it takes place successfully only through assiduous attention given to the matter over the medium to longer term. Ideally this should be achieved smoothly over time and without development of aggravations, though this cannot always be guaranteed.
This article does not have the space in which to set out any details of the available range of detoxifying diets. Suffice it to say that the most profound errors and imbalances of the British diet (or the American or Northern European diet) should be addressed and eliminated. That means excluding or at least minimizing added salt and sugar, keeping fat intake to not more than 20% of calorie intake, avoiding frying and other sources of fat that has been heated in air and keeping protein intakes adequate but modest, ensuring adequate amounts and balance between Omega 6 and Omega 3 fatty acids. If one wants to go further, one would avoid wheat and dairy products during the detoxification period. For a period of detoxification lasting, say, three months, a vegan diet that is wholly or mainly organic vegetables, pulses and rice, with the pulses not exceeding 60g/day, will provide an excellent background intake. Longer periods of detoxification will require a programme to permit more liberal choice.
7 You do not have to use a Special Diet to Benefit
The above dietary suggestions apply to the ideal situation where the subject is willing to comply fully with the best recommendations. However, one of the most important points about detoxifying nutrients is that they can benefit anybody. Anyone who eats the typical British diet, awful though that is from any naturopathic standpoint, will be far better off using detoxifying nutrients than not using them. The toxins that accumulate due to excessively high protein intake (e.g. big meat-eaters) will be best detoxified if the person has a good supply of the detoxifying nutrients. The same will be true of the person who eats many meals from fish and chip shops or other forms of fatty fast food outlets or take-aways.

Again, if you have your health condition compromised through excessive salt and sugar in the diet at least your body will have a light at the end of the tunnel if you supply it with detoxifying nutrients. Bear in mind that the British diet is often not high in these nutrient requirements. When the diet is either highly toxic or toxifying and is also short in the detoxifying nutrients, then you have the worst of both worlds.
Therefore an approach that involves supplementing the detoxifying nutrients can even benefit people who are quite determined not to improve their typical British eating habits.
8 Detoxification Inadequacy Causes Chronic Illnesses
According to the old naturopaths, detoxification failure is a final common pathway to most, if not all, forms of chronic illness.
Certain of the chronic illnesses have been the subjects of scientific evidence that links their cause to failure of detoxification mechanisms. These include Parkinson's disease, chronic fatigue syndrome (ME), fibromylagia, cancer, irritable bowel syndrome and multiple chemical sensitivities. Yet formal scientific investigation of the relationship between detoxification inadequacy and the causes of chronic illnesses has barely got under way. Most workers in this field expect that many more such connections will be discovered. If one is permitted to extrapolate a little from what we already know it seems quite likely that, just as the old naturopaths said, detoxification failure is a final common pathway to most, if not all, forms of chronic illness. An exception to this may be illnesses that are specifically genetic (e.g. porphyria, alcaptonuria or phenylketonuria) in which an enzyme is deleted through an inborn genetic error. These deletions cause in each case an error of metabolism other than a detoxification error. However, even the detoxification adequacy of an individual is partly controlled by genes, as we see below.
9 Detoxification Ability and Genetics
Many of the detoxification enzymes are said to be "polymorphic". This term means that they exist in different versions, some of which work better than others. To make the matter personal, this means that if we consider any one from among the whole battery of such enzymes, the version that we possess can be a top class version, indifferent or else a poor one. You can draw "a long or a short straw".
Medical drugs of the synthetic chemical variety are quite correctly regarded as toxins to the body and it will come as no surprise to learn that before we can get rid of them, they have to be metabolized by detoxifying enzymes. As you would expect, people with known detoxification inadequacy are more than usually prone to suffer adverse reactions to drugs. Different classes of medical drug have to be detoxified by different detoxifying enzymes. Depending upon which enzymes of one's body are less than adequate, one may be prone to adverse reactions towards different classes of drugs.
If you happen to draw a short straw in relation to one or more of your important detoxifying enzymes then this may make you more prone to one or more of the serious chronic illnesses. An example of this is Parkinson's disease, which is more than usually likely to occur in individuals having a lower grade version of the gene CYP2D6. The function of this gene is associated with detoxification adequacy. If you have a poor version of it then clearly the reduced ability to detoxify certain classes of toxin may result in early death of those groups of brain cells that are involved in Parkinsonism. However, possession of such a lower grade gene does not necessarily condemn the person to have Parkinsonism. Evidence to date suggests that there are about 35 genes in the human genome that affect detoxification adequacy. Unfortunately if you have a genetic disadvantage that affects your ability to detoxify, there is nothing you can do to alter that situation. But you can make allowance for it, as the next section will show.
10 How to Compensate for Genetic Disadvantage
Given that genetic disadvantage exists (and it has to be admitted that most people do not know whether they have it or not), then the other factors that affect detoxification performance are environmental and dietary. Environmentally, one should minimize toxin exposure. It is arguable that everyone should do so, but it is clearly more important for those with a detoxifying disadvantage. That calls for attention to the quality of drinking water, the use of organic food and minimizing exposure to chemicals of all types, including those chemicals, like garden and household chemicals that other people may handle freely. Dietary precautions, apart from eating from organic sources, include reduction of protein and fat levels within an adequate range (as already mentioned) and eating a combination of foods and supplements that will provide the specific nutrient requirements for detoxification. Obviously your disadvantaged enzymes will work better if the cells are encouraged to produce more of them and if they are well supplied with their co-factors and substrates. This can at least be a partial compensation for genetic disadvantage.
11 How can one find out about Genetic Disadvantage?
To have a genetic assessment for oneself of the 35 genes for detoxification adequacy would be quite a substantial project and is hardly practical for most of us. However, one can rely upon a fairly well tried approach that involves challenging the body with a toxin to observe how well the body transforms and excretes the toxin. The caffeine test is an example. A known dose of caffeine is administered and the body treats it as a toxin. Measurement of the amount of detoxified caffeine produced is a measure of detoxifying ability. The same can be done with benzoic acid as a test substance. The body converts it to hippuric acid by linking it to the amino acid glycine. Measuring the hippuric acid produced again constitutes a test of detoxifying ability. The limitation is that each of these tests is specific to a particular group of enzymes and that other tests have to be devised for other enzymes.
12 How Should One Develop a Detoxification Strategy?
1. The main thesis of this article is that one's detoxification ability should be augmented by nutrients that support the detoxifying enzymes. Therefore, whether these are in a composite formulation or taken as separate nutrient supplements this action should be the first plank in the strategy. These nutrients are fully listed in the last section of this article.
2. Modify the diet. Get away from the worse excesses and imbalance of the UK or western diet. Follow the guidelines for this outlined in section 6 above. It would be better still to obtain professional help from a well trained, holistic nutritional practitioner.
3. Consider using a herbal bowel cleanse either before or at the same time as using the special nutritional supplements recommended.
4. Use a good quality bowel flora preparation comprising acid-producing species, especially Lactobacilli and/or Bifidobacteria.
13 Reviewing the Detoxifying Enzymes
As mentioned above, detoxifying a chemical toxin usually involves two phases. The first phase is most often an oxidation. As that name implies this is a reaction that adds oxygen. There are some technical variations upon that definition but the principle that oxygen is involved in the reaction is valid. Where toxic molecules are concerned, the most common reaction is one that adds an oxygen-containing group, which is the (-OH) group, called the hydroxyl group. This reaction type is therefore termed a "hydroxylation". These reactions are usually carried out by enzymes of a special class called the "P450 cytochromes". These are by far the most important Phase I enzymes in the body. These enzymes are distinguished by the fact that they are pigmented. The reason for this is that they contain haem, the same pigmented material that colours the blood red. Haem contains iron as a component and this fact gives us the first nutritional connection with detoxification. Without iron you cannot have P450 cytochromes. "Cytochrome" means "cellular pigment". Typically then, these enzymes convert the toxic molecule into a derivative having an additional -OH group. This effects a chemical change and the toxin is no longer the same substance. It is usually less toxic than the original toxin, though that is not an invariable rule. In any case, it retains toxicity and in most cases that makes it imperative that it should be removed quite quickly from the cell. The -OH containing toxin derivative is a product of Phase I detoxification and it can usually be removed only by the operation of Phase II.
In Phase II the Phase I product is chemically bonded to another molecule and that bonding almost always results in a significantly less toxic derivative. This "joining" reaction at Phase II is distinguished by the term "conjugation". The substance that is joined to the Phase I product has to be of a special kind. These "joining" molecules are called "ligands". There are several of these, among which are the amino acid glycine, the sugar derivative glucuronic acid and sulphate. Obviously the Phase II enzymes require a generous supply of these ligands. This is the second nutritional point. Ligands must be provided either by converting other tissue constituents or, more directly, by nutritional intake of suitable ligands. This very important sequence of Phase I and Phase II is represented in the diagram below.
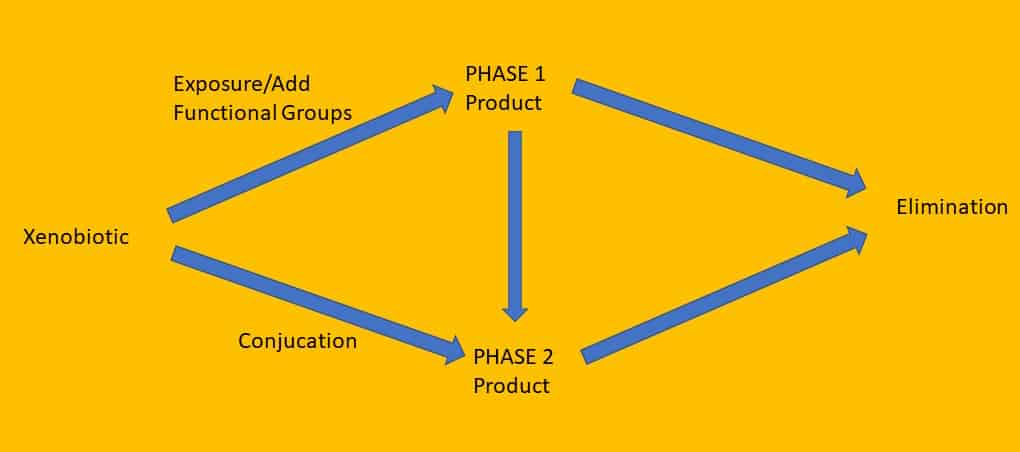
Figure I
We also have to be aware that there are variations of the above general scheme that apply to particular toxins. They do not quite all fit into exactly the same pattern. One such variation involves bypassing Phase I altogether, so that only Phase II is required. In that case we have a simplified scheme.
Other variations that apply to some individual toxins or toxin types involve somewhat different kinds of Phase I reaction, although Phase II follows in the familiar way. These variations are as follows.
1. An important functional group on the toxin molecule may be "masked". That means it is "covered over" by another group attached to it. The Phase I reaction may involve removing the masking group to expose the previously hidden function group.
2. The Phase I reaction may involve formation of an epoxide group. These are "epoxidations".
3. The Phase I reaction may involve removal of alkyl groups that may have been added by toxic alkylating agents. These are "dealkylations".
4. The Phase I reaction may involve removal of amino groups. These are "deaminations".
5. The Phase I reaction may involve removal from the molecule of atoms of the group of elements called "halogens", usually, chlorine or fluorine. These are "dehalogenations".
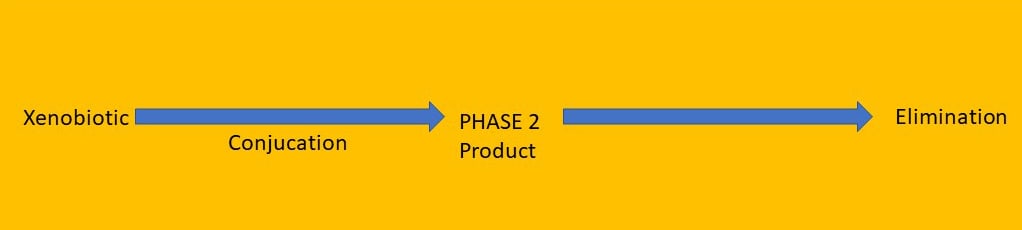
Figure 2
For non-chemist readers the nature of these reactions may not be grasped, but they are all Phase I reactions and the point being stressed here is that while addition of an -OH group may be typical, it is not invariable.
It is stressed here too that in just a few significant cases, the Phase I reaction may lead to a modified toxin product that is much more toxic than the original toxin. Obviously these represent a particular danger. The Phase I biochemical system has clearly evolved because it bestows a great survival advantage to the organism. However, the enigma of Phase I is that the range of possible toxins that may beset the organism is vast and virtually limitless. No system could be designed to "foresee" them all and provide for each one individually. Therefore the Phase I system that has evolved is not without the possibility of errors. The error that can occur is that a few special toxins may, more or less accidentally, get though the Phase I transformation with a still more potent toxicity. This is true, unfortunately, of quite a few of the potent carcinogens. These come into the body only mildly carcinogenic but are transformed by the body's detoxifying enzymes into potent carcinogens. If they were living things, one might be tempted to ascribe to them the evolution of a way to evade the detoxifying mechanisms. Of course, the truth is that they are non-living chemical molecules but, nonetheless, their variations of chemical structure succeed in getting them through the first phase of the human detoxifying system, not merely unchanged, but actually with enhanced destructive potency. However important are these exceptions to the rule, do note that they are exceptions and that most toxins are reduced in toxicity by Phase I.
There are distinct nutritional strategies that enhance Phase I mechanisms and other nutritional strategies that enhance Phase II. The lesson we must learn from the above is that it would be counter- productive to follow a strategy for stimulating Phase I only. In some cases this would leave us exposed to highly toxic Phase I products that are ready to be conjugated and detoxified in Phase II. But if we have not provided the nutrients for Phase II then we shall be exposed to the full destructive effects of the Phase I products.
We now need to look at these biochemical steps in more detail and to focus upon their nutritional requirements. However one does this, one has to probe into the biochemistry of detoxification. This involves naming the toxins and the enzymes that handle them. The next part of the article therefore contains far more technical detail than the above. Out of it comes a quite full specification of the nutritional needs for an ability to detoxify well.
14 Detoxifying Toxins by Oxidation - Cytochromes P450
This group of enzymes comprises a huge number of different but related types and is referred to often as a "super family". The unifying features are the similarity of the reactions being catalyzed and the fact that they are all haem proteins. They also bear some similarity to another group of enzymes that are also cytochromes present in the mitochondria of the cell. These are part of the respiratory chain and involved in oxidizing foodstuffs to generate the energy of the cell as ATP. However, for all the similarity, this mitochondrial function is very different from detoxification. Moreover the cytochrome P450 family is located, not in the mitochondria but in the very fine membranous structures within the cytoplasm of the cell, called the endoplasmic reticulum.
The substrates for P450 cytochromes (the substances upon which they work) can be fatty acids, steroids and, most particularly, a huge range of foreign substances (foreign toxins) including medical drugs. Of 10 mammalian families of P450s, six are associated with steroid metabolism, one with fatty acid metabolism and three with the metabolism of foreign compounds. Among the latter, the most diverse family, family 2, contains at least eight subfamilies each having from 1 to 12 members. The probability is that there are more P450s still to be found than the number now known. It has even been estimated that in rodent liver the P450s make up some 20% of all the protein of the endoplasmic reticulum. Need anyone doubt the major role of the liver in detoxification reactions?
The fact that there are hundreds of different cytochrome P450 enzymes serves to emphasize their importance in the cell's "economy". It would appear that there has to be so many different kinds to allow for a very wide range of foreign toxins that the cell might encounter.
Among the many drugs reported as substrates for cytochromes P450 are phenobarbital, morphine, ethylmorphine, codeine, paracetamol, and amphetamines. Among other foreign toxins are the notorious carcinogens, ethylcholanthrene and benzpyrene, as well as aminopyrine, nitro-compounds, aniline, azo dyes, benzene, carbon tetrachloride. An additional dietary component metabolized by cytochrome P450 is alcohol and an additional physiological substrate is squalene, an intermediate in steroid synthesis.
15 The Effects of Nutrition upon Cytochromes P450
There are many interactions between diet and nutrition and the activity of the P450 system. An example of a diet-related connection is that with polyunsaturated fat. Today most people are well aware of the need for polyunsaturated fat in the diet of both the Omega 3 and Omega 6 types to promote health. However, their highly reactive double bonds need protecting against oxidation. When too much polyunsaturated fat is consumed without sufficient anti-oxidant protection the endoplasmic reticulum is exposed to peroxidation of its lipids through free radical attack. P450 cytochromes may be inactivated in that process (Tien et al., 1981).
A diet too high in total fat stimulates the production of increased cytochrome of the type P450IIEI (Yoo et al., 1991). This is one member of the family known to activate carcinogens and thereby to promote mammary, colonic, pancreatic and pulmonary cancers in animals (Imaida et al., 1989). Hence, relatively low fat diets with adequate but not excessive polyunsaturated fatty acids would seem to be indicated. This control of fat intake would be the best solution but the adverse effect of diets too high in total fat is also reversible, at least in the rat, by adding sufficient dietary fibre.
The cytochromes P450 need to be regenerated after the reaction by co-enzymes that are in part derived from nicotinamide, and therefore from Vitamin B3. These work together with a flavoprotein enzyme that requires riboflavin (Vitamin B2). Thus the B vitamins involved in detoxification.
Rogers & Newberne (1975) showed that detoxification of foreign toxins in the endoplasmic reticulum of the cell required lipotrophic nutrients, i.e. nutrients required for the synthesis of phospholipids and biological membranes. These consisted of choline, glycine, folic acid, Vitamins B6 and B12, polyunsaturated fatty acids and phosphate. Lu et al. (1974) showed that phosphatidyl choline was specifically needed for full activity of the cytochromes P450. Deficiency of choline was shown to lead to lipid peroxidation and auto-oxidative liver damage in rats within days and to induce liver cell cancer in more than half of the animals in two years. These effects could be prevented by simultaneous administration of free radical scavengers (Ghoshal et al. 1990). Also, dietary deficiencies of choline and methionine in the rat much increased the carcinogenic effect of ethylnitrosamine in the animals’ livers (Sawada et al. 1990).
Vitamin C is also essential for the oxygenation of foreign toxins by cytochrome P450. Vitamin E too plays an essential role by protecting the membrane of the endoplasmic reticulum from peroxidation. Vitamin A was also shown to have a strong effect upon P450s, there being 30% less of them in Vitamin A deficient rats compared to supplemented controls (Colin et al., 1991). The role of riboflavin in the enzyme (NADPH-cytochrome reductase), with which P450s have to work, has been mentioned. However, research exists showing that the effect of riboflavin deficiency upon this system and its hydroxylating activity can be fairly crucial (Yang, 1974). On the other hand, thiamine deficiency (Vitamin B1) leads once again to excessive production of the especially undesirable cytochrome P450IIEI, with toxic effects. Clearly, for good detoxification either riboflavin deficiency or thiamine deficiency should be avoided.
The role of iron as a component of the P450s has been mentioned. Whilst one cannot form P450 cytochromes without iron, there is probably no need to supplement iron unless there is manifest clinical deficiency of the mineral.
Magnesium is another mineral that enhances P450s and their associated reductase enzyme. It encourages the cell to maintain good levels of these active enzymes. This may be due to protection against peroxidation and / or by maintaining good concentrations of glutathione to ensure adequate free radical quenching (Hsu et al., 1982).
This provides us with a strategy for maintaining the Phase I enzymes at a good level of activity. Apart from dietary measures, supplementary choline, glycine, folic acid, Vitamins B6 and B12, polyunsaturated fatty acids, Vitamins B1, B2 and B3 may well be needed, along with magnesium and Vitamin A. One has a choice between providing ready-made phosphatidyl choline or free choline.
16 Nutritional Effects upon Other Oxidative Enzymes
Superoxide dismutases are part of the cell's defence against free radicals. These enzymes need zinc, copper and manganese. Glutathione peroxidase needs selenium and, indirectly, nicotinamide and catalase needs iron. Hence a connection is already made between detoxification and the need for these nutrients. Full adequacy of these nutrients is recommended to maintain fully functional levels of these detoxifying enzymes.
17 Detoxifying Toxins by Conjugation - Associated Nutritional Requirements
Just as hydroxylation of foreign toxins enhances their solubility and decreases their toxicity in most cases, Phase II detoxification reactions occur by conjugation. Conjugation is a word that signifies a "joining together". These linkages are made primarily to glucuronic acid, sulphate, acetyl, glutathione or the amino acid glycine. These are the "ligands" already mentioned. The toxin substances being conjugated may or may not have been already hydroxylated by the cytochromes P450.
Conjugates with glucuronic acid (glucuronides) are very important in detoxification. The glucuronic acid is derived from glucose and does not have to be taken in ready-made. The bile pigment bilirubin (a breakdown product of haemoglobin) is detoxified in this way, as are thyroid hormones and many drugs, chemicals, such as phenol, and environmental pollutants. Alcohols, phenols generally and carboxylic acids (most organic acids) undergo this fate. The reaction is carried out in the endoplasmic reticulum by enzymes called glucuronyl transferases. These enzymes require as a co-factor uridine, which is one of the nitrogen bases present in RNA. This does not have to be taken in ready-made either but we have to be sure that the co-factors involved in synthesizing uridine are provided.
However, less obviously, Vitamin C has been shown to play a very significant role and hence the glucuronyl transferase enzymes are low when Vitamin C is deficient. Vitamin C continues to justify its reputation as a gentle supporter of detoxification processes. The glucuronyl transferase enzymes (i.e. linkage to glucuronic acid) apparently provide quantitatively the most important single route for detoxification of environmental chemicals in mammals, and by implication, in humans (Neumann & Zannoni, 1990). Hence it would be hard to put forward a nutritional detoxification programme that did not include Vitamin C.
Other substances are detoxified via conjugation with sulphate. In some instances the same substance may be detoxified in part with glucuronide and in part with sulphate. The reaction takes place in the cytosol (the liquid part of the cell contents). Conjugation with sulphate requires the sulphating coenzyme. This has a formidable name, doubtless meaningless to non-chemists. For those who want to know it is PAPS (3'-phosphoadenosine-5'- phospho-sulphate). The enzymes involved are the sulphotransferase enzymes. Nutritionally, the sulphation process is prone to shortage of its specific ligand, sulphate (Levy, 1986). Therefore we must include sulphate or sources of sulphate into any nutritional programme designed to stimulate Phase II. It is usual to provide this by means of sulphur amino acids, especially cysteine, or dietary sulphate may be used. Even when the dietary supply of sulphur amino acids is normal deficiency may occur through circumstances that create an abnormal demand upon the body's sulphur reserves. One of these occurs when there is cyanide in the diet, such as may be caused by consuming uncooked cassava, especially when the season is dry and the cassava has a high cyanide content.
The cyanide is detoxified mainly by conversion to the less toxic thiocyanate and requires an input of sulphur. This sets up a high sulphur demand, leaving insufficient for the sulphation detoxification pathway. The enzyme that does this (Rhodanese) is another detoxifying enzyme, specific to cyanide, but it competes directly with the Phase II sulphation enzymes for the body's limited sulphur supplies.
Naturally, the situation is made worse by a diet of plants with many naturally occurring toxic chemicals and a high requirement for glutathione. Thus the nutritional demands of the different detoxification pathways can interact and they can compete for scarce nutritional resources. This problem has been reviewed by Parke (1993b). Adequate intake of the sulphur amino acids, cysteine and methionine, is clearly to be recommended. Toxic substances detoxified mainly or partly by sulphation are again some alcohols and phenols, the drug, paracetamol and the female hormone oestradiol.
Another form of enzymic detoxification is conjugation with one or more acetyl groups, derived from acetic acid. Like sulphation the reaction occurs in the cytosol. It is carried out by two or more "acetyl transferase" enzymes that draw upon a form of acetyl that is widely available within the cell, namely acetyl co-enzyme A. That involves pantothenic acid (Vitamin B5). Humans vary in their ability to detoxify by acetylation and divide into "fast and slow acetylators". They vary accordingly in the way in which they detoxify and the rate at which they detoxify some drugs. Primary amines and hydrazines are examples of substances usually handled by this route. Drugs susceptible to this route include the antibacterial sulphonamides, such as sulphanilamide and sulphadiazine, the antituberculosis drug isoniazid and the anti-hypertensive drug acetylhydrazine.
A conjugation reaction of huge importance in detoxification is the one with glutathione (GSH). The nature of glutathione and its role in free radical scavenging have been described above. The conjugation reactions of glutathione involve linking the toxin to the -SH group (sulphydryl group) of the glutathione through the actions of enzymes called glutathione-S-transferases. We can employ the use of coffee enemas used in as they are specific stimulators of the glutathione-S-transferases of the liver. Hence, the coffee enema impacts upon the patient's detoxifying enzymes to effect an improvement of activity.
Toxins typically detoxified in this manner include polycyclic hydrocarbons, arsenic, acetaminophen, heavy metals such as lead, peroxides and aflatoxins, e.g. from the moulds growing on peanuts. Similar reactions occur with lindane, methylmercury, atrazine, methyl iodide, 3,4- dinitrobenzene, benzyl chloride, diethylmaleate, naphthalene, transtilbene oxide (TSO), the epoxide of vinyl chloride and 1,2-epoxyethylbenzene. It must be stressed that these are only examples and that this enzyme system is clearly adapted to handle a very wide range, indeed, of potential and actual foreign toxins. These enzymes are located primarily in the cytosol, with far lower levels present in the endoplasmic reticulum. They are ubiquitous among the body tissues, not just the liver, with the greatest activity in the testes, liver, intestine, kidney and adrenal gland. There are four families of these enzymes, controlled by four separate groups of genes. As with the P450 families, these display different abilities to handle toxins of different kinds.
The nature of the detoxification route that is initiated by glutathione-S-transferases is that the conjugation with glutathione comes first, followed by removal of the glutamic acid and glycine portions of the glutathione molecule. This leaves behind a toxin-cysteine conjugate. Addition of an acetyl group to this leads to a "mercapturic acid", which is a water- soluble detoxification product and readily excreted by the kidney.
More and more research studies are serving to emphasize the vital roles played by glutathione and the relatively parlous and relatively defenceless position of the human body that is deprived of normal tissue concentrations of it. It is a highly protective metabolite. This is important, because in many chronic and pre-chronic states, glutathione levels slump and oxidative stress results. After all, glutathione has three separate roles in detoxification - the glutathione peroxidase route, the conjugation route and a key role in regenerating Vitamin C. Nutritionally, the importance of glutathione further emphasizes the essentiality, for adequate detoxification, of the dietary sulphur amino acids, cysteine and methionine.
Interestingly, it is possible to augment tissue levels of glutathione by dietary intake of the ready-formed compound (Reicks & Hathcock, 1988). Whilst glutathione is available from supplement suppliers, it is not widely used for that purpose on account of its high cost and because other cheaper nutritional measures can be adopted to safeguard tissue glutathione levels. In particular there are strong indications of Vitamin C's involvement, along with bioflavonoids like quercetin, in maintaining the tissue levels of glutathione. The quercetin connection places emphasis upon the use of onions in the diet as a good quercetin source. Vitamin C, as glutathione's "right hand man", can produce indirectly a benefit similar to that of giving glutathione itself. Hence, the body's defences against oxidative stress and toxins appear to be "integrated" and various components of the system depend upon others.
Tissue glutathione levels were shown by Kubow et al 1985 and Kubow & Bray 1988 to be highly crucial in protecting against lung injury in goats, more so than either Vitamin E or free cysteine.
Halliwell (1993) picks out glutathione depletion for emphasis. Writing of free radicals he says:
"These species have been implicated in over 100 conditions, from arthritis and haemorrhagic shock to AIDS. In the latter disease, attention has focussed on GSH depletion (and subsequent oxidative stress) as a consequences of HIV infection." And "This wide range of diseases implies that ROS are not something esoteric, but that their increased formation accompanies tissue injury in most, if not all, human diseases".
"R O S" stands for "reactive oxygen species" and means the same as "free radicals". Moreover, there is evidence that a genetic lack of one particular species of glutathione-S-transferase enzyme (neutral GST) is linked to a special susceptibility to lung cancer (Seidegard et al., 1986). This sort of evidence, that connects a lack of detoxification power with susceptibility to chronic illness, is being gathered progressively. It can also be noted that in cataract patients the concentration of reduced glutathione in the lens tissue is below normal. Further, in a study of the serious nutritional deficiency, kwashiorkor, the children who died were those with the lowest tissue levels of glutathione, glutathione peroxidase, zinc and Vitamin E (Golden & Ramdath, 1985).
Other forms of conjugation include reaction with the amino acids. For example, in forming the bile salt, cholic acid is conjugated with the oxidized sulphur amino acid taurine to give taurocholic acid. Benzoic acid is conjugated with glycine to give hippuric acid and phenylacetic acid is conjugated with glutamic acid to give phenylacetylglutamine. Finally, a special high sulphur protein, metallothionine, is specialized to bind toxic heavy metals such as cadmium. It is not quite a conjugation reaction, but similar.
18 Practical Action
The benefits of a detoxifying diet and avoidance of environmental toxins have been stressed already. Other practical action depends upon the use of nutritional supplements to supply the substrates and co-factors for the detoxifying enzymes and to ensure that high levels of detoxifying enzymes are produced and maintained. Such supplements should include realistic levels of Vitamin E, Co- enzyme Q10, Vitamin C, Vitamin A, Glutathione, Selenium, Nicotinic acid, Choline, Glycine, Folic acid, Vitamin B6, Vitamin B12, Riboflavin, Thiamine, Magnesium, Sulphate, Zinc, Cysteine, Methionine, Glutamic acid, Manganese and Copper.
In view of the special properties of carotenoids in free radical quenching, it is also recommended that naturally sourced beta-carotene, alpha carotene, lutein and lycopene be included at levels that make a genuine difference. Iron would be needed in addition if there was any reason to think the person was iron- deficient. It would be a most favourable development if a single formula could be developed that would offer all these ingredients. It would greatly improve the prospect of individuals who need detoxification enhancement actually taking the necessary steps. Such a formula would need to avoid the common pitfall of the nutritional industry of providing levels that "look OK on the label" but which are actually inadequate to perform any real physiological function.
19 How to use this Article
This article is not intended as individual medical advice to the reader, but is provided more generally for information. Individual patients wishing to detoxify often do undertake self-designed programmes on their own responsibility. The best route, however, is to opt for the advice of a fully trained nutritional practitioner and that is to be recommended.
20 References
Blake, D.R., Allen, R.E. & Lunec, J. "Free radicals in biological systems - a review orientated to inflammatory processes", British Medical Bulletin, 43 (2) 371-385 (1987).
Colin, C., Narbonne, J.F., Migaud, J.L., Grolier, P., Cassand, P. & Pellissier, M.A. "Lipid peroxidation and benz(a)pyrene activation to mutagenic metabolites: in vivo influence of vitamins A, E, C and glutathione in both dietary vitamin S sufficiency and deficiency" Mutation Research 246 159-168 (1991).
Golden, M.H.N. & Ramdath, D. "Free radicals in the pathogenesis of kwashiorkor". In Proceedings of the XIII International Congress of Nutrition, (Eds. Taylor, T.G. & Jenkins, N.K.) John Libbey, New York, pp597-598 (1985).
Halliwell, B. "Oxygen radicals as key mediators in human disease: fact or fiction?", in "Food, nutrition and chemical toxicity" Ed. Parke, D.V., Ioannides, C. & Walker, R., Smith Gordon, Chapter 12 (1993).
Hsu, J.M., Rubenstein, B., & Puleker, A.G. "Role of magnesium in glutathione metabolism in rat erythrocytes", Journal of Nutrition 112 488-496, (1982).
Imaida, K et al., "Enhancing effect of high fat diet on 4-nitroquinoline 1- oxide-induced pulmonary tumorigenesis in ICR male mice", Japanese Journal of Cancer Research 80 499-502 (1989).
Institute for Functional Medicine Inc., "Detoxification: A Clinical Monograph", Gig Harbour WA USA (1999).
Kubow, S & Bray, T.M. "The effect of lung concentrations of glutathione and vitamins on the pulmonary toxicity of 3-methylindole", Canadian Journal of Physiology and Pharmacology 66 863-867 (1988).
Kubow, S., Bray, T.M. & Janzen, E.G. "Spin-trapping studies on the effects of Vitamin E and glutathione on free radical production induced by 3- methylindole", Biochemical Pharmacology 34 1117-1119 (1985).
Levy, G., Sulfate conjugation in drug metabolism: role of inorganic sulphate", Federation Proc. 45 2235-2240 (1986).
Lu, A.Y.H., Levin, W., & Kuntzman, R. "Reconstituted liver microsomal enzyme system that hydroxylates drugs, other foreign compounds, and endogenous substrates. VII. Stimulation of benzphetamine N-demethylation by lipid and detergent" Biochemical and Biophysical Research Communications 60 266-272. (1974).
Lunec, J. "Free radicals: their involvement in disease processes", Ann. Clin. Biochem. 27 173-182 (1990).
Neumann, C.M., & Zannoni, V.G. "Ascorbic acid deficiency and hepatic UDP- glucuronyl transferase. Qualitative and quantitative differences" Biochemical Pharmacology 39 1085-1093 (1990).
Parke, D.V., Ioannides, C. & Walker, R., Eds., "Food, nutrition and chemical toxicity" Smith Gordon, Chapter 39 419-426 (1993a).
Parke, D.V. "The mantakassa epidemic", in "Food, nutrition and chemical toxicity" Ed. Parke, D.V., Ioannides, C. & Walker, R., Smith Gordon, Chapter 39 419-426 (1993b).
Reicks, M. & Hathcock, J.N. "The effects of methionine and other sulphur compounds on drug conjugations" Pharmacology and Therapeutics 37 67- 79 (1988).
Rogers, A.E. & Newberne, P.M. "Dietary effects upon chemical carcinogenesis in animal models for colon and liver tumours" Cancer Research 35 3427- 3431 (1975).
Sawada, N., Poirier, L.,Moran, S., Xu, Y-H. & Pitot, H.C. "The effect of choline and methionine deficiencies on the number and volume percentage of altered hepatic foci in the presence or absence of diethylnitrosamine initiation in rat liver" Carcinogenesis 11 273-281 (1990).
Seidegard, J., Pero, R.W., Miller, D.G. & Beattie, E.J. "A glutathione transferase in human leukocytes as a marker for the susceptibility to lung cancer" Carcinogenesis 7 751-753 (1986).
Tien, M., Suingen, B.A. & Aust, S.D. "Superoxide-dependent lipid peroxidation" Federation Proceedings of the Federation of American Societies of Experimental Biology 40 179-182 (1981).
Yang, C.S. "Alterations of the aryl hydrocarbon hydroxylase system during riboflavin depletion and repletion" Archives of Biochemistry and Biophysics 160 623-630 (1974).
Yoo J.S.H., Park, H.S. Pantuck, C.B., Pantuck, E.J. & Yang, C.S. "Regulation of Hepatic microsomal P450 IIEI level by dietary lipids and carbohydrates in rats" Journal of Nutrition 121 959-965 (1991).